💊 New skin cancer treatment more effective than expected
A new combination of drugs proves effective against advanced skin cancer, according to a three-year clinical study. Half of all participants showed a complete response, and after one year of treatment, 80 percent of participants survived.
Share this story!
A clinical study for a new drug combination for advanced skin cancer, intended to stop the deterioration of the immune system that occurs in some of the patients, has proven effective, the University of Colorado announces on its website.
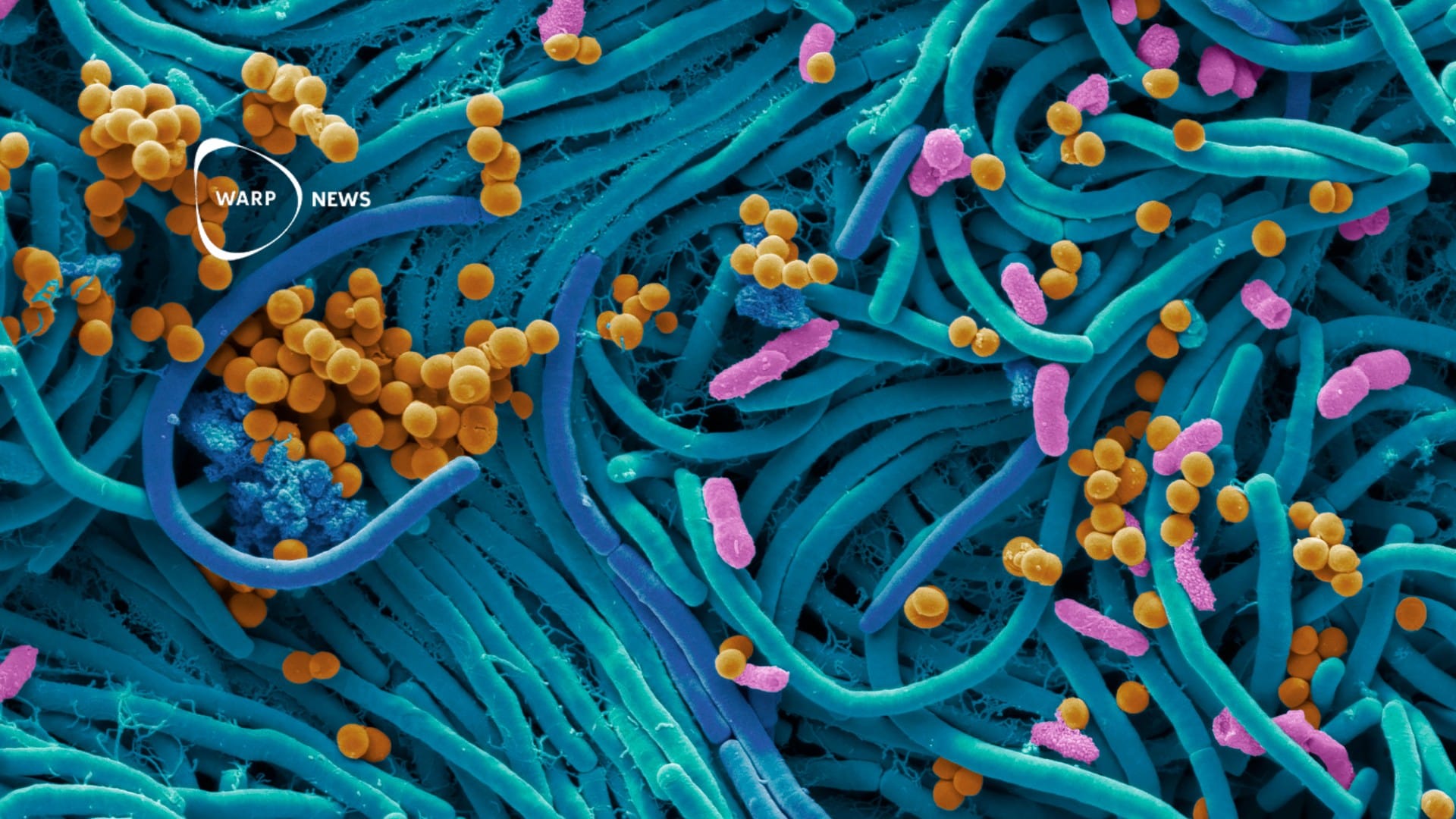
The study was done on patients with advanced skin cancer and focused on cases where immunotherapy does not work, something that happens when the cancer suppresses the immune system, thus preventing the effectiveness of that kind of treatment.
The study used a combination of two drugs, the immunotherapy treatment pembrolizumab (Keytruda), which approximately 40 percent of patients respond to individually. Combined with the chemotherapy treatment all-trans retinoic acid (ATRA), which targets the cells that suppress the immune system, the number of patients who responded to the treatment increased to 71 percent, half of whom recovered completely from the disease.
A good news that ATRA proved to be effective in this context, according to Martin McCarter, research leader in the study, is that ATRA has minimal side effects. The drug does not contribute to increasing the toxicity of the treatment; the most common side effect is a headache that disappears as soon as the treatment is over. Thus, the results are very promising for those patients who have not responded to immunotherapy.
Results worth celebrating
The researchers are now celebrating the results of the study, which proved to be more effective than expected. From the beginning, they suspected that the results they would achieve were on par with the treatments already available. That they managed to target the oppressive cells, according to McCarter, had been a victory in itself. But beyond that, the patient response was stronger than expected.
“You dream about stuff like this. You work so hard on science, but just like in the startup world, 95 percent of things like this fail. Despite all one's best intentions or all the best science that looks like 'this will work', when you transition to humans, it usually doesn't work. So to see a hypothetical mechanism like this actually work, and you see it actually help patients, that's why we're in this business,” says McCarter.
Now the clinical study is expanding to more patients, who have not responded to other types of immunotherapy. Having shown that the method is both safe and effective, it is the only direction to travel in, according to McCarter, as it is the patient group that needs the most help right now.
By becoming a premium supporter, you help in the creation and sharing of fact-based optimistic news all over the world.